A 75 year old male with swelling over abdomen and pain over the swelling
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
A 75 year old male, farmer by occupation, came to OPD with chief complaints of swelling over the abdomen since 5 years and pain over the swelling since 15 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 5 years ago and then he noticed a swelling over his epigastric region, insidious in onset, size of a peanut which gradually progressed to the present size. There is no relation to standing, walking or straining. It was slightly reducible to lying down. No aggravating and relieving factors. Patient also complained of pain over the swelling since 15 days, which was sudden in onset, non progressive, stabbing type of pain, no radiation of pain. No aggravating or relieving factors. Patient had increased work load before 15 days for almost a month.
No history of trauma, chronic cough, shortness of breath, constipation, loose stools, vomiting, fever, cold, burning micturition. No history of chest pain, palpitations, orthopnea, PND.
DAILY ROUTINE:
He wakes up around 4am, goes to the bathroom, freshens up, gets milk from the farm and takes his breakfast. He takes roti with milk mostly as breakfast and goes to work. He finishes his work by 12 in the afternoon and goes back home to have his lunch. He then takes a nap and wakes up at around 4pm and spends time with his family and relatives until dinner. He sleeps at around 10pm.
PAST HISTORY:
No similar complaints seen in the past.
Not a known case of Diabetes Mellitus, Hypertension, Tuberculosis, Epilepsy, Thyroid disorders, CAD etc.
Surgeries: Patient has a history of ESWL for left renal calculi.
Drugs: Uses painkillers for his knee pains every once or twice a week for two days. He got checked for his knee pains, it turned out to be just wear and tear of cartilage due to his old age. Not on any other medications.
FAMILY HISTORY:
No similar complaints seen in the family.
PERSONAL HISTORY:
Diet is mixed, Appetite is normal, Sleep is adequate, Bowel and Bladder movements are regular. No known allergies. Patient was a chronic smoker (chutta) from the age of 11, takes toddy (1 bottle). He reduced his intake from 3 years and takes it occasionally now. Last consumption was 1 month ago.
GENERAL EXAMINATION:
Patient was conscious, coherent and cooperative. Well oriented to time, place and person. Well built and nourished.
There are no signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy, generalised edema.
Vitals:--- BP: 110/70mmHg PR: 80bpm Temp: afebrile RR:18cpm
SYSTEMIC EXAMINATION:
Per abdomen:
On Inspection, Shape of the abdomen is round, flanks are free, Umbilicus is centrally placed, inverted. A solitary swelling noticed in the epigastric gastric region of the size 4*3cm, oval in shape, smooth, well defined margins, skin over the swelling and around the swelling is normal,moving with respiration. Scars of vaccination, done in his village, present on either sides of the umbilicus. sinuses, visible pulsations, dilated veins seen. No pigmentation.
On Palpation, all inspectory findings confirmed except the size being 5*3cm. No local rise of temperature. Tenderness present only at the site of swelling that is in the epigastric region. Cough Impulse is not present. Liver and spleen not palpable. Kidney not palpable.
On Percussion, dull note present over the swelling, tympanic note heard in other areas. No fluid thrill or shifting dullness.
On Auscultation, Bowel sounds heard (7/min)
CVS: S1,S2 heard, No murmurs, thrills, heeves.
Resp: BAE + NVBS +
CNS: No neurological focal deficits are seen.
PROVISIONAL DIAGNOSIS:
Epigastric Hernia...?
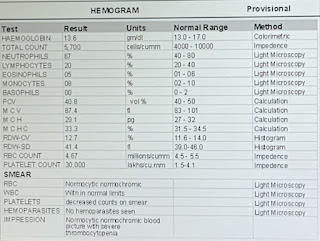
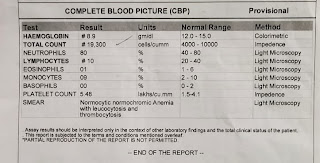
INVESTIGATIONS:
Random blood sugar: 170mg/dl
Total bilirubin: 0.97 mg/dl
Direct bilirubin: 0.2 mg/dl
SGOT: 10 IU/L
SGPT: 10 IU/L
PROVISIONAL DIAGNOSIS:
Chronic ITP…?
TREATMENT:
1. IV fluids- NS @ 50ml/hr
2. Monitor vitals 4th hourly
3. Input/Output charting




















Comments
Post a Comment