A 60 year old female with pain, vomiting and burning micturition
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
A 50 year old female patient, fruit seller by occupation, came to casualty with chief complaints of abdominal pain since 15 days; vomiting since 15 days; burning micturition since 15 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 15 days back then she developed abdominal pain in the epigastric region, which was of squeezing type, associated with vomitings, food as content, black in color, non projectile, non bilious, non foul smelling, 3-4 episodes. It was not associated with fever, nausea, giddiness, loose stools. She also had burning micturition, frothy urine, urgency, polyuria, nocturia. No history of polydypsia.
DAILY ROUTINE:
Patient wakes up around 6am, does household chores and takes rice and curry as breakfast. She then sits outside the house, selling fruits there. She takes rice and curry for lunch then she takes an afternoon nap. She wakes up and takes rice and curry for dinner. She sleeps around 9pm.
PAST HISTORY:
No similar complaints seen in the past. Patient is a known case of diabetes since 20 years, hypertension since one year. She is also a known case of TB five years back. No history of CAD, epilepsy, asthma and thyroid disorders.
Patient has a history of split skin graft for right diabetic foot 4 years back. History of left below knee amputation, 1 year back. History of hysterectomy on 4th march 2022 (1 year back).
FAMILY HISTORY:
No similar complaints seen in the family. Her mother is a known case of diabetes.
PERSONAL HISTORY:
Diet is mixed, appetite decreased, sleep is adequate, bowel and bladder movements are regular. No known allergies. No addictions.
DRUG HISTORY:
She takes mixtard insulin 20 units SC/od since 20 years for diabetes. She aslo takes Telma 40 and Amlo 5mg po/od. History of blood transfusion 8 units.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative. Well oriented to time. Thin built and moderately nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy and edema.
Vitals: Temp: afebrile BP: 130/90mmHg PR: 86/min RR: 18/min GRBS: 398mg/dl SpO2: 98%
SYSTEMIC EXAMINATION:
Per abdomen examination:
On Inspection, the abdomen is obese, flanks are free, umbilicus is transverse. There was striae present and a vertical line present down from umbilicus (hysterectomy scar),no presence of sinuses, puncture marks on skin, linea nigra, visible pulsations, dilated veins.
On Palpation, all the inspectory findings are confirmed. Tenderness present at epigastric region. No local rise of temperature. No hepatomegaly and spleenomegaly. Kidney palpable by bimanual palpation.
On Percussion, every region is resonant.
On Auscultation, bowel sounds heard.
Cardiovascular: S1, S2 heard Respiratory: NVBS + no added sounds CNS: NAD
PROVISIONAL DIAGNOSIS:
Pancreatitis..?! Gastric ulcer..?!
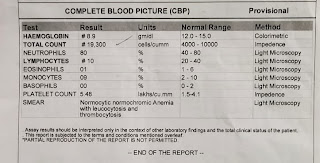
INVESTIGATIONS:
TREATMENT:
1. NBM till further orders
2. IVF. NS @75ml/hr
3. INJ. PIPTAZ 2.25gm
4. INJ. TRAMADOL 1 AMP in 100ml NS
5. INJ. OPTINEURON 1 AMP in 500ml NS
6. INJ. PAN 40mg IV/OD
7. INJ. ZOFER 4mg IV/SOS






Comments
Post a Comment