A 75 year old female with SOB
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
A 75 year old female patient, housewife, was brought to casualty with chief complaints of shortness of breath since 10 days, weakness since 4 days and decreased appetite since 4 days.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 5 years back and then she developed shortness of breath and was taken to a private hospital where she was diagnosed with bronchial asthma and was treated with nebulisation.
Shortness of breath seasonal variation (every year during winters)
Patient developed similar complaints with fever and was admitted in a private hospital, treated as bronchial asthma 6 months back.
10 days back, she developed shortness of breath (grade 3- MMRC grading) which was insidious in onset, gradually progressive, associated with cough (non productive) and fever.
SOB not associated with chest pain, chest tightness, palpitations, sweating. No history of orthopnea, paroxysmal nocturnal dyspnea, headache.
Symptoms were relieved with medication nebulisation.
4 days back patient developed increased shortness of breath (grade 4- MMRC), weakness, increased fatigue, decreased appetite, unable to move from bed or walk without support.
4.12.2022- She was taken to miryalguda hospital with increase severity of SOB and weakness. Investigated and referred here (KIMS- narketpally).
PAST HISTORY:
Patient had a history of fall (head injury) 10 years back, which was not associated with loss of consciousness, projectile vomiting, seizure, weakness of limbs. Neuroimaging of brain was done. She was then diagnosed with hypertension and was started on Telma H. 4 years back, patient was also diagnosed with hypothyroidism (not on any medication)
Patient is not a known case of Diabetes, cardiovascular disorders, TB, epilepsy.
DAILY ROUTINE OF PATIENT:
Patient wakes up at around 6am, eats her breakfast made by one of her family members. She has her own room. Lunch around 1pm includes rice and vegetable curry or dal. She does not eat snacks, for dinner it is rice and curry at around 8pm.
Patient's lifestyle is sedentary with minimal physical activity (only walks around the house)
FAMILY HISTORY:
Not significant.
PERSONAL HISTORY:
Diet is vegetarian, appetite is decreased, sleep is adequate, bowel and bladder movements are regular. No addictions. No known allergies to pollen, dust.. Patient is on Telma H for hypertension. Tab.Montelukast (OD) and Tab. prednisone (OD) daily for 5 years.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative. Well oriented to time, place and person. Thin built and malnourished.
Pallor +
No icterus, cyanosis, clubbing, lymphadenopathy, pedal edema
Vitals: Temp: afebrile PR: 80bpm irregularly irregular BP:100/60 mmHg GCS: E2V5M6 RR: tachypneic SpO2: 98% on 2litres of O2 GRBS:132mg/dl
SYSTEMIC EXAMINATION:
Respiratory system:
Inspection: Shape of chest is elliptical. Bilateral symmetrical chest. Trachea appeared to be central. Expansion of chest is equal on both sides, No accessory muscles of respiration are used. No drooping of shoulders. No wasting of muscles. Supraclavicular hollowness seen on the right side. Apical pulse not seen.
Palpation: All inspectory findings are confirmed. No local rise of temperature. No tenderness. Trachea is central. Chest expansion equal on both sides. Tactile vocal fremitus is equal on both sides. Chest circumference: 72cm
Percussion:Resonant in all areas
Auscultation: BAE + VBS Crepts heard on inspiration and expiration in infraaxillary region. Rhonchi heard at infra axillary and infra scapular.
Cardiovascular system: Apex beat auscultated at 5th intercostal space. S1 and S2 are heard. No murmurs.
Central nervous system: Oriented to time place and person.
Motor: Power 4/5 in both sides of upper limbs and lower limbs. Tone normal
Reflexes: bilaterally biceps 2+ triceps 2+ supinator 2+ knee 2+ ankle 2+
Sensory: Pain, touch, temperature and pressure +
Per Abdomen: Shape is scaphoid. No organomegaly. Bowel sounds heard.
PROVISIONAL DIAGNOSIS: Acute exacerabation of asthma, COPD? miliary TB? ILD?
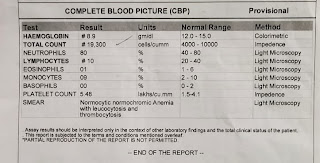
INVESTIGATIONS
CBP, CXR PA view, HRCT..
ECG: sinus rhythm irregular MAT?
Chest X ray: Pleural thickening, Fine reticular interstitial suggesting of ILD
HRCT: yet to be taken..
MANAGEMENT:
O2 inhalation with 2-4l/min
inj. augmentin
inj.pantop
nebulisation with duolin
hypokalemia and hyponatremia under evaulation














Comments
Post a Comment