A 60 year old male with SOB and fever.
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
A 60 year old male, labourer by occupation, resident of Siripuram, came to casualty with chief complaints of shortness of breath since 2 months, fever since 1 week.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 months ago, then he developed shortness of breath which was insidious in onset, grade IV (MMRC). It was not associated with orthopnea and PND. It was not associated with any chest palpitations, chest tightness. Patient also had fever,intermittent, associated with chills and rigors, moderate, insidious in onset, gradually progressive, no aggravating factors, relieved temporarily on medications. There is history of night sweats. There is no history of cold, cough, nausea, vomiting. There is history of back pain, facial puffiness since 2 months. There is history of decreased urine output, hesitancy, urine was of pale yellow type There is history of pedal edema since 2 months, extending up to knee, no aggravating factors, relieved on walking. No history of diarrhoea, constipation.
PAST HISTORY:
No similar complaints seen in the past. Patient is a known case of hypertension since 8 years and is on telma.H. Patient is also a known case of diabetes mellitus I since 6 years and is on sitagliptin. Patient is not a known case of TB, asthma, epilepsy, CAD, thyroid disorders.
FAMILY HISTORY:
No similar complaints seen in the family.
PERSONAL HISTORY:
Diet is mixed, appetite is decreased, sleep is adequate, bowel movements are regular, urine output is decreased, hesitancy. No known allergies. Non smoker and does not consume alcohol. Not any kind of medications
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative. Well oriented to time, place and person. Moderately built and moderately nourished.
There is edema of feet. There is no pallor, icterus, cyanosis, clubbing, lymphadenopathy.
Vitals --- BP: 130/90 mmHg PR: 82 bpm Temp: afebrile RR: 16 cpm
SYSTEMIC EXAMINATION:
Per abdomen:
On Inspection, shape of abdomen is flat, flank fullness is not present. No scars, sinuses, hernial orifices, dilated veins, visible pulsations. Umbilicus is centrally placed, inverted. No pigmentation.
On Palpation, all inspectory findings are confirmed. No local rise of tenderness. NO tenderness. Liver and spleen are not palpable.
On Percussion, no fluid thrill or shifitng dullness.
On Auscultation, bowel sounds are heard.
CVS: S1S2 heard; no murmurs heard
Resp: NVBS + BAE +
CNS: NAD +
PROVISIONAL DIAGNOSIS:
CKD..?
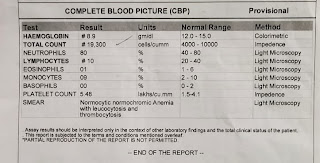
INVESTIGATIONS:
TREATMENT:
1. TAB.NICARDIA 16mg PO/BD
2. TAB.OROFER PO/BD
3. INJ.EPO 4000 IU/SC once weekly
4. INJ.HAI S/C TID
5. SYP. CREMAFFIN 15ml PO/HS
6. TAB.ECOSPIRIN 75mg PO/HS
7. TAB.TORSEMIDE 100mg PO/BD
8. TAB.CLONIDINE 0.1mg PO/OD
9.TAB.BISOPROLOL 25mg PO/OD
10. Salt restriction <2gm/day
11. Fluid restriction <1.5 lit/day













Comments
Post a Comment