A 60 year old male with abdominal distention and pain abdomen
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
A 60 year old male, labourer by occupation, resident of Kodad, came to casualty with chief complaints of abdominal distention since 3 months, pain abdomen since 3 months.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 3 months ago, then he developed abdominal distention which was insidious in onset, gradually progressive with tightness present. It aggravates on taking food and there are no relieving factors. It is also associated with shortness of breath which aggravated on taking food. No associated orthopnea and paroxysmal nocturnal dyspnea. Patient also had abdominal pain since three months which was insidious in onset, gradually progressive. It was diffuse, cramping type and no radiation. It aggravated on taking food and no relieving factors. Patient has loss of appetite, weight loss. There are no associated symptoms like diarrhoea, constipation, fever, nausea, vomiting, flatulence, belching, hiccups, heartburn, pedal edema, loose stools, indigestion. There is no history of burning micturition, altered urinary output, chest tightness, palpitations, night sweats. No foetus, flatus, feces. History of jaundice two years ago, used herbal medication. History of similar complaints three months ago and ascitic tap was done.
PAST HISTORY:
History of jaundice two years ago; used herbal medication. Patient is not a known case of DM, TB. Hypertension, asthma, epilepsy, CAD and thyroid disorders.
FAMILY HISTORY:
No similar complaints seen in the family.
PERSONAL HISTORY:
Diet is mixed, appetite reduced, sleep is adequate, bowel and bladder movements are regular. He consumes alcohol from two years but discontinued from 5 months ago. No smoking. No known allergies.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative, well oriented to time, place and person. poorly built and moderately nourished. No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy and edema.
temp: afebrile PR: 92/min RR: 17cpm BP:110/70mmHg SpO2: 98%
SYSTEMIC EXAMINATION:
Per Abdomen:
On Inspection, Shape of abdomen is round, flank fullness is present. No scars, sinuses, dilated veins, visible pulsations. The umbilicus is centrally placed and slightly everted. Skin is smooth. No pigmentation.
On Palpation, all inspectory findings are confirmed. No local rise of temperature. Tenderness present all over the abdomen. Abdominal girth: 87 ----> 82cm
On Percussion, shifting dullness present, fluid thrill is not present.
On Auscultation, bowel sounds are heard.
CVS: S1S2 heard, no murmurs heard
Resp: NVBS+ BAE+
CNS: NAD +
PROVISIONAL DIAGNOSIS:
Chronic liver disease..?
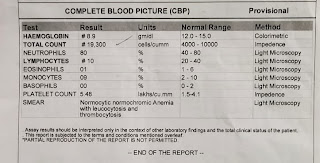
INVESTIGATIONS:
TREATMENT:
1. Fluid restriction <1.5L/Day
2. Salt restriction <2g/Day
3. Protein powder 2 scoops in 1 glass of water/ PO/BD
4. T.LASIX 20mg/PO/BD
5. SYP>LACTULOSE 15ml/PO/SOS
6. SYP.HEPAMERZ 10ml/PO/BD
7. Daily abdominal girth and weight monitoring.
















Comments
Post a Comment