A 45 year old male with pain abdomen and vomitings
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
A 45 year old male, carpenter by occupation, resident of Chityal, came to OPD with chief complaints of pain in the abdomen since 3 days and vomitings since 1 day.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 3 days ago and then developed pain in the epigastrium region, sudden in onset, non progressive, no aggravating factors but relieves on bending forward, pain radiating to his back along the left side. No giddiness, pedal edema, SOB. Patient also complains of vomitings since 1 day, 3 episodes since yesterday, contains food materials, non bilious, non projectile. Stools not passed since two days. No history of cough, cold, fever, diarhhoea, nausea.
PAST HISTORY:
There are no similar complaints seen in the past. Patient is not a known case of diabetes, hypertension, TB, epilepsy, CAD, thyroid disorders.
FAMILY HISTORY:
No similar complaints seen in the past.
PERSONAL HISTORY:
Diet is mixed, appetite is decreased, sleep is adequate, bladder movements are regular, constipation is present (two days since stools passed). No known allergies. Non smoker. He consumes alcohol everyday since 15 years, 2 quarters of alcohol per day, last binge of alcohol consumption is two days ago (6 april'23). Not on any kind of medications.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative. Well oriented to time place and person. Moderately built and moderately nourished. Pedal edema is present, non pitting type. No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy.
Vitals --- BP: 110/80 mmHg PR: 76 bpm Temp: afebrile (97.8 F) RR: 18 cpm
SYSTEMIC EXAMINATION:
Per abdomen:
On Inspection, shape of abdomen is scaphoid, flank fullness is present. No sinuses, hernial orifices, dilated veins, visible pulsations. Umbilicus is centrally placed, inverted. No pigmentation.
On Palpation, all inspectory findings are confirmed. No local rise of tenderness. Tenderness present in the epigastrium region. Liver and spleen are not palpable.
On Percussion, shifting dullness is present, no fluid thrill.
On Auscultation, bowel sounds are sluggish (2/min)
CVS: S1S2 heard; no murmurs heard
Resp: NVBS + BAE +
CNS: NAD +
PROVISIONAL DIAGNOSIS:
Acute pancreatitis...? Gastric ulcer...?
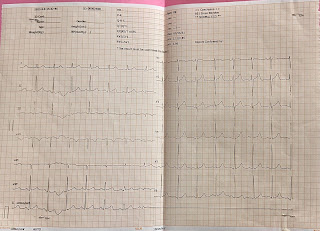
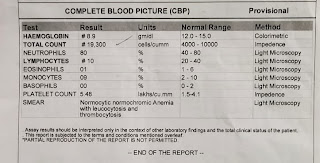
INVESTIGATIONS:





Comments
Post a Comment