Rheumatoid arthritis case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
A 59 year old female patient came to orthopaedics department with chief complaints of pain in the left pelvic bone since two months.
History of present illness: The patient was apparently asymptomatic three years ago, then she was infected with chikungunya and was on meds for ten days, to treat the Arthralgia in her fingers. Later she developed pain in her right hip bone and found out that she had rheumatoid arthritis because she had not used the medications given for chikungunya on time and that’s what caused this. She underwent surgery i.e total hip replacement for her right pelvic bone in Yashoda hospitals, Hyderabad. Then two months back, she developed the same pain in her left hip bone which was throbbing type of pain along with burning sensation. It was not a radiating type of pain. The patient is unable to bend or move properly. There is no h/o fall. No swelling seen at the site of pain
Past history : Patient is not a known case of hypertension, diabetes, thyroid diseases, CVD, epilepsy. Surgeries: THR for right pelvic bone
Family history: No significant family history
Personal history: Diet is mixed, low appetite, sleep is adequate, bowel and bladder movements are regular. Patient regularly takes toddy from 20 years, once every three days. Last taken: four days before date of admission (3/3/20). No known allergies.
Drug history: On ulcer protectives since three months
General examination
Patient is conscious, coherent and cooperative. Well oriented to time place and person. Moderately built and nourished
No pallor, icterus, cyanosis, clubbing, lymphadenopathy and Oedema
Vitals: BP:130/70mmHg regular rhythm and normal volume PR: 92/min regular , normovolemic afebrile, RR: 14 cycles/min
Systemic examination
CVS: S1,S2 +. RS: normal breath sounds heard.
CNS: NAD
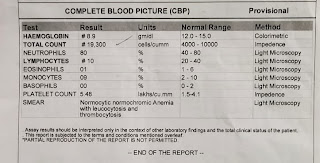
Investigations
Urea: 20mg/dl
Creatinine: 0.7
Na: 141 K: 3.4
High ESR and CRP
Rheumatoid factor: negative
ANA: negative
Provisional diagnosis: Rheumatoid arthritis
Treatment: surgery- THR on left hip bone
Post surgery:
Current medications:
Inj. Pantoprazole 40mg iv
Inj. Ceftriaxone iv/im
Paracetamol infusion 100mg/100ml







Comments
Post a Comment